This is Everlee. This is her story, and how she is battling her severe case of X-Linked PVNH.
She was born 7/27/21, 373 days ago, and has spent a majority of her life living in a hospital bed.
At 2 days old, we had no idea that a CT would change her life forever. When the doctors noticed a spot on her forehead bulging out whenever she cried, they decided to do a CT to see if it was just cosmetic. Thankfully it was, however they found something else. They sent her for an MRI, and consulted neurology to come and talk to us because they found gray matter all over her ventricles in her brain, which they confirmed was bilateral periventricular nodular heterotopia. They instantly began getting in contact with genetics to figure out the cause. They took her blood, and we had to wait the long journey for answers.
In the nicu her o2 dropped on several occasions, but our concerns were ignored, even though she appeared faintly blue around her mouth. We were told she was fine, and that she was just cold, and I still wish to this day we would’ve pushed harder…We went home from the nicu with hope, thinking no big deal, she has PVNH, this just means she could maybe have seizures one day, but not likely until in her 20s. And then 4 weeks went by, she wasn’t stooling easily on her own at home, her hernia became bigger and more concerning, and she started rolling and fluttering her eyes in a weird way. Her neurologist instantly booked for her to have a 24 hr eeg stay at the hospital. Once at the hospital, hooked up to monitors they found her o2 dropping again, and I told them about her nicu experience. Instantly we weren’t there for just an eeg anymore.
They ran every test under the book; echo, ekg, eeg, ultrasounds, x rays, and lastly a 12 hour apnea test. It wasn’t seizures, the only thing They found was that she had a small PDA, that they felt wasn’t contributing to the oxygen issues, and that she had periodic breathing apnea. After 10 days, they sent her home on 1/8 of a liter of oxygen. She continued to the next several months to require more and more oxygen, they found her periodic breathing was actually severe obstructed sleep apnea, she kept getting illness after illness from respiratory to gastric, her weight declined rapidly and she could not take in more than 2.5 oz every 4 hrs of formula, she began having awful retching and vomiting , and was started on meds for severe GERD, she was below the 1st percentile for her weight. They did a triple Endoscope procedure on her (laryngoscopy, bronchoscopy, endoscopy) to see if there was any inflammation in her stomach or airway causing infection, and to see if she could have an interstitial lung disease causing the oxygen issues, and it came back fine. We saw a surgeon who stated her hernia was fine for now, and he gave us tools to use for rectal dilation to help her stool.
At her 4 month check up in November, during her routine exam, her pediatrician listened to her and I could tell something was wrong. And she said “I hear a murmur”, her cardiology follow up in regards to her small PDA wasn’t for another month, but she was able to move it up to the following week. At that appointment we learned her PDA had grown, and was now moderate in size, she was experiencing slight L to R shunting and it was now causing a murmur. That’s when they realized the hole was not gonna close itself and they began discussing surgery. We didn’t know why all of this was happening to our little girl… and then 4 days after her cardiology appointment, we got the call from genetics.… Everlee’s PVNH was being caused by filamin A with the FLNA gene. It explained everything.
And then the answers started to slowly come together in 2022. After several weeks in December of battling with more severe weight issues, us, and her PCP, GI specialist, and her surgeon agreed a G tube was best. She had the surgery on the 3rd of January, as well as a nissen fundoplication for the GERD. Even with that, her GERD continued to be intense, after a swallow study and upper GI and looking back on her triple E they found that she has a level 1 laryngeal cleft, causing intense laryngeal penetration, with risk for aspiration. After her unfortunately getting aspiration pneumonia from her continuing to vomit, they switched her to a GJ tube. She is unable to tolerate anything more than a couple necessary meds to her stomach (g tube). In fact, she has to drain all of her stomach contents (bile, gas bubbles/air) 24/7 into a drain bag, and her feed bypasses the stomach and goes to her intestines (J tube). She has continued to have illness after illness, from rhino virus to gastritis to C DIFF from antibiotics given to treat a different infection
She’s had paraflu, rhino enterovirus, E. coli, gastroenteritis, pneumonia, coronavirus Hcov43, the list goes on. Her heart procedure had to be pushed back 2, almost 3 times. In March we obtained a second opinion at CCHMC cardiology, and with their own findings, and more experience with FLNA, they confirmed she has moderate pulmonary hypertension, and she had begun to have mitral valve regurgitation. Her PDA was very large and she was shunting more severely. They wanted to close her PDA themselves, and so we planned to return their a month later in April for the procedure. She had other plans…

2 weeks later she was admitted to ACH again, and she slowly got worse and worse until they determined she was in pulmonary hypertension crisis. She was life flighted to CCHMC and had her PDA closed 4 days later. While still intubated after, they got a CT of her chest, which showed her right lung had almost completely collapsed. She has battled with under developed areas of the lungs for months but they never came to a diagnosis for the cause. While at Cincinnati they got her second opinions on all her issues and rapidly more diagnoses and answers flooded in. They confirmed her to have pulmonary hypoplasia, and bronchomalacia due to the FLNA, and they also diagnosed her developmental delays and low muscle tone to be from cerebral palsy brought on by the brain damage that the PVNH has caused.
She is 13 months old and does not sit up on her own, she doesn’t roll over, and holding her own head up is tremendous work. They started her on more meds for suspected gastroparesis and dysmotility, and she is on an extensive bowel regimen. They ran tests and confirmed she has a redundant colon and she has malpositioning of her cecum. She sees her motility team in a couple weeks to discuss surgery to do full motility studies on her. She is up to 2 full liters of oxygen now to this day, and she cannot go even 5 minutes without oxygen support. She is still battling her weight, she still sits below the 1st percentile at only 13 lbs 15 oz, but we are hoping the motility studies will key in some more answers on why she can’t gain weight but she can with TPN support when admitted to the hospital. On June 10th she was admitted to ACH again, with sick like symptoms, same as every time before. Vomiting foamy white fluid, wheezing, etc. She was taken by squad, and in the ER was admitted to the regular floor, we got the results from all her labs early the next morning, and it was RSV….something we had been told, would be deadly if she got it… Within 40 hours the medical response team was paged and she was emergently rushed to the picu where her airway collapsed from the malacia right as they got there, luckily they were able to get her hooked up to higher flow oxygen (vapotherm) and she stabilized. She was doing better for a couple days, but she wasn’t able to wean off the high flow, and into her regular nasal cannula o2, which is something we found odd.
On June 15th, at 6 pm respiratory checked her, scored her breathing, and said she looked good, but was wheezing so they decided against attempting to wean. By 6:30 everything was not fine. She had a stridor, there was no signs of her breathing any air out of her body. People kept flooding in the room, they put her on CPAP ventilation support and it wasn’t doing anything to help her, her palliative team came and sat with me and asked me all the painful questions about extraordinary measures, they were administering epi, and preparing a crash cart. The doctor reached out to several specialists in pulmonary, and other picu attendings, because he knew the risk of intubation with someone with FLNA, and how easy it is to become dependent on that support, especially with someone with as bad of lungs as Everlee. She had a huge chance of becoming dependent on it, and needing a trach, or worse…not surviving at all. But there was nothing else to do, and time was out, she was minutes from arresting. So they intubated her.
After they intubated her they ran tests and found that her entire airways, and a majority of her lungs had completely collapsed. The only “open” parts of her lungs were the lower lobes on both sides, and those are the areas that are already underdeveloped as it is, from the hypoplasia. She was intubated for 12 days, and in those 12 days her lungs continued to just open up, and then collapse again. Over and over. She developed MRSA in her throat and lungs on top of everything. She was medically paralyzed in a coma so she couldn’t move. She was placed on her stomach for several days because even with the ventilator breathing for her, she couldn’t hold her o2 up unless she was prone. That’s the first time I’ve ever seen her tolerate tummy time, and it was heart wrenching in those conditions….She was on every sedative in the book, several antibiotics, steroids, meds for her lungs, she was on TPN for 3 weeks. They were reaching out to Cincinnati to see about their opinions on traching her, because they knew with FLNA she could require that to begin with one day. We had reached the point of gathering specialists to form a family meeting to discuss our options moving forward. And then a miracle happened out of nowhere…
Everlee took a turn for the better, and was able to wean from all her medications, and was able to be woken up, and she stopped fighting the intubation. She SMILED over the tube in her mouth and started to take breaths over the vent. They tried Spontaneous breath trials, and she passed , and continued to pass them every 6 hrs when they did them, and so they put her on steroids for airway swelling, and on the morning of June 27th, at exactly 11 months old, and on her great grandfathers birthday (he passed away just 3 months before she was born last year), Everlee was extubated! She skipped CPAP support and went straight to high flow, and within 40 hrs she was weaned off high flow and back to her base line of 2 liters of standard o2 support. She went back to the regular floor a couple days later and within 8 days post extubation- She was off TPN, and was discharged, back HOME, healthy.
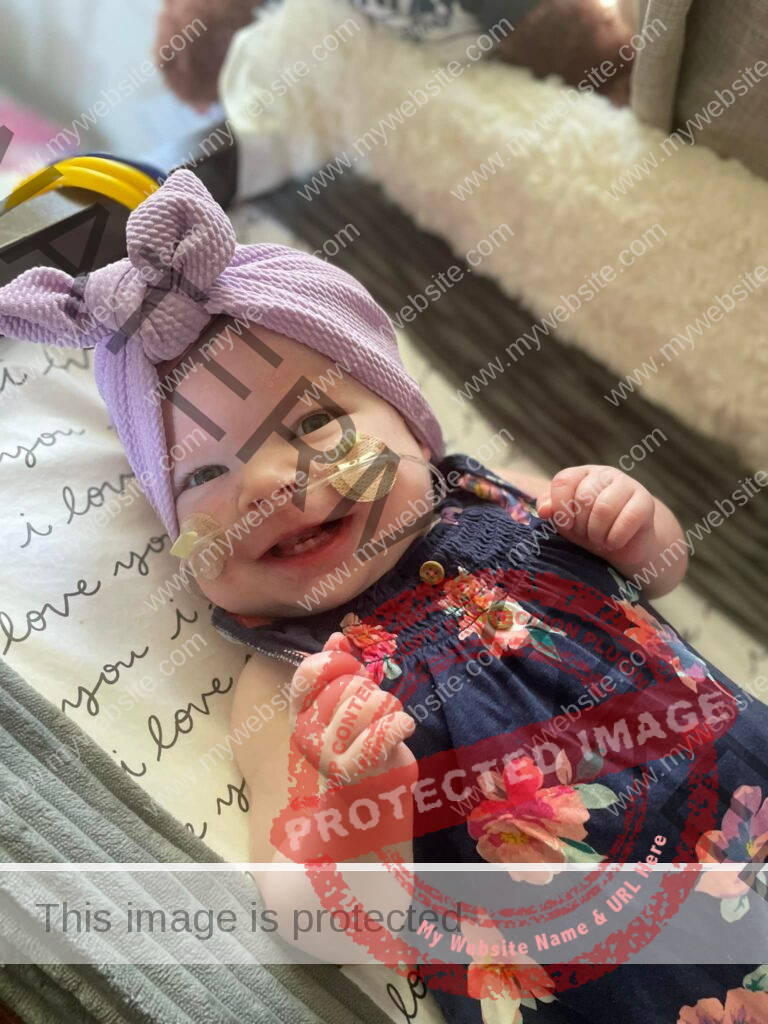
And now, as of tomorrow, she will have been home for an entire month. A RECORD for her home time (she has gone 16-18 days between hospital admissions the last 9 months). She is slowly gaining weight, she is about to be fitted for her kid kart wheelchair, and she sees all of her specialists in Cincinnati in just a couple weeks, where we hope to gain more answers, and less bad news. She still has a lifetime of struggles ahead, they say atleast a lung transplant or trach is likely in her future. She is nowhere near eating or walking on her own, and we don’t know what will happen in the seizure department down the road, she will likely develop them, as most FLNA patients do…but we will face the storm one rain drop at a time. She is our miracle, we can’t quite wrap our heads around why things happen, and how she made it out alive and trach free, or why things are starting to look up now… Some people have said “maybe that was her body’s rock bottom” But we sure love her to absolute pieces.
If you are still with me reading, I appreciate you very very much. Please, follow her journey below to keep up to date on how she’s doing, and always always, pray for her little life.
Everlee’s Elaborate Journey#PVNHsupport #MarchOnPVNH #PVNH #PVNHawareness #pvnhlife #rarediseaseawareness #XLinkedPVNH #FLNA #FilaminA
Carlee, Everlee’s mom
Everlee’s Elaborate Journey#PVNHsupport #MarchOnPVNH #PVNH #PVNHawareness #pvnhlife #rarediseaseawareness #XLinkedPVNH #FLNA #FilaminA


